Lyme Disease 101
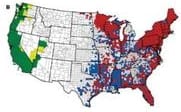
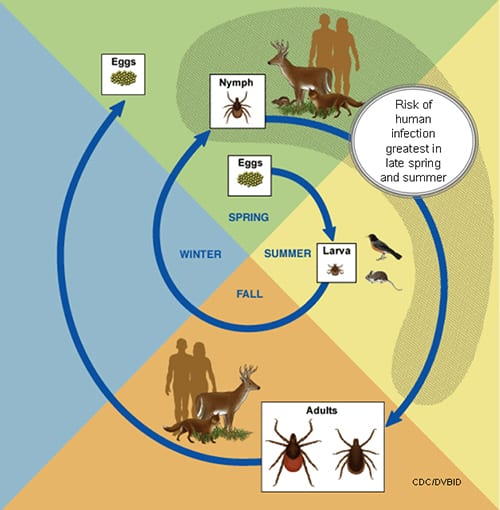
Minnesotans across the state are at risk for acquiring tick-borne diseases. The highest risk is in the southeast, east central and north central areas of the state. Grassy fields, brush-filled wooded landscapes and places where residential neighborhoods meet the forest edge are prime tick habitat. Our brochure contains information to help you mitigate your risk for Lyme and other tick-borne diseases.
Blacklegged Ticks in 49% of U.S. Counties

Life Cycle of Blacklegged Tick
CDC
Preliminary estimates released by the Centers for Disease Control and Prevention indicate that the number of Americans diagnosed with Lyme disease each year is around 300,000. read more
MN Dept. of Health
If a patient has an EM highly suggestive of Lyme disease and recent symptom onset (<2-3 weeks), B. burgdorferi antibody tests are not recommended because of low sensitivity at this stage of infection. Read More